https://doi.org/10.52733/KCJ21n2-cs2
ABSTRACT
Novel immune checkpoint inhibitors (ICI) have yielded remarkable response rates in metastatic renal cell carcinoma (RCC), including sarcomatoid RCC (sRCC). Here, we show the feasibility and efficacy of robotic-assisted cytoreductive partial nephrectomy (cPN) following a remarkable response to combination ICI for metastatic sRCC in a young female. A female in her late 40s presented with poor-risk, metastatic sRCC emanating from a 6.5 cm left renal mass including pulmonary involvement, retroperitoneal lymphadenopathy, and a scalp metastasis. She received 4 cycles of combination ipilimumab and nivolumab followed by maintenance nivolumab with a remarkable and durable response. Given the apparent downstaging of her primary tumor, a robotic cPN was pursued for residual ypT1aN0R0 sRCC and found to be both feasible and safe with exceptional perioperative outcomes. She has since done well clinically and oncologically. Our unique case of metastatic sRCC in a young female highlights several aspects pertinent to the contemporary management of metastatic RCC including the role for cytoreductive nephrectomy in selected patients, the safety and feasibility of a nephron-sparing and minimally-invasive approach to cytoreduction after downstaging with ICI, and remarkable sensitivity of sRCC—a classically aggressive entity—to ICI. Insights: We present a unique case highlighting the role for cytoreductive nephrectomy in selected patients with metastatic renal cell carcinoma (RCC), the safety and feasibility of a nephron-sparing and minimally-invasive approach to cytoreduction after downstaging with immune checkpoint inhibition (ICI), and remarkable sensitivity of sarcomatoid RCC—a classically aggressive entity—to ICI.
INTRODUCTION
INTRODUCTION
The role of cytoreductive nephrectomy for metastatic renal cell carcinoma (mRCC) continues to evolve in the contemporary immunotherapy era,1,2 and the efficacy of cytoreductive partial nephrectomy (cPN) is even less well-described. Novel immune checkpoint inhibitors (ICI) have yielded unprecedented response rates in mRCC, including sarcomatoid RCC (sRCC),3,4 one of the most aggressive entities of RCC. Here, we describe the feasibility, safety, efficacy, and durability of robotic-assisted cPN and regional retroperitoneal lymphadenectomy in a young female who demonstrated a remarkable response to combination ipilimumab and nivolumab for metastatic sRCC.
CASE PRESENTATION
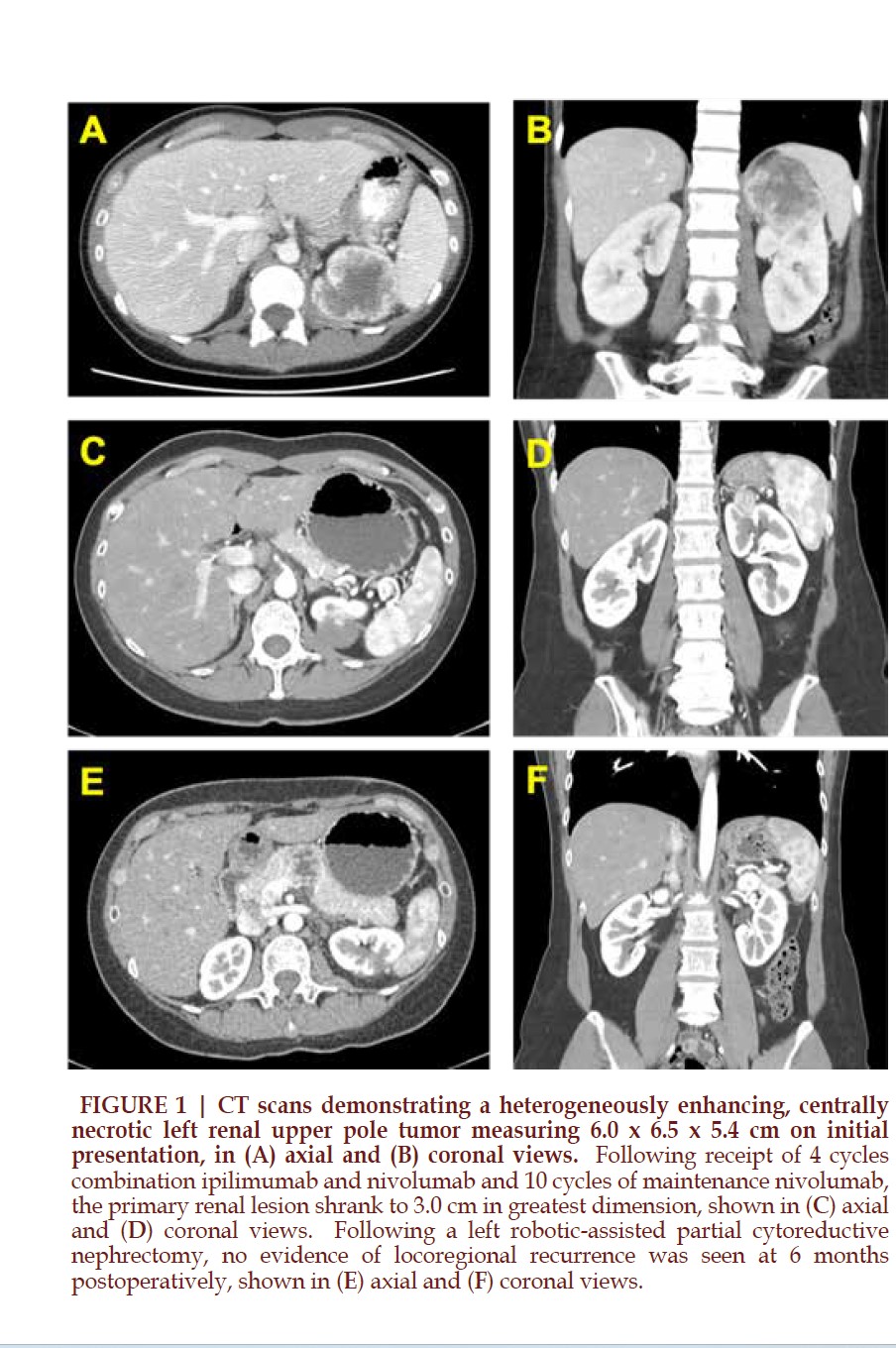
A healthy Asian woman in her late 40s with excellent functional capacity presented to her gynecologist with abdominal pain, night sweats, unexplained weight loss, intermittent palpitations, and dry mouth. Laboratory evaluation revealed anemia and hypercalcemia. CT imaging of the chest, abdomen, and pelvis revealed a dominant 3.8 x 2.5 cm irregular, heterogeneously enhancing left upper pulmonary lobe perihilar soft tissue mass, multiple small pulmonary nodules, enlarged retroperitoneal lymph nodes, and a 6.0 x 6.5 x 5.4 cm solid, heterogeneously enhancing, centrally necrotic left renal upper pole mass concerning for a primary renal malignancy (Figure 1A and 1B).
The patient was also noted to have a scalp mass, for which she underwent a biopsy that revealed an infiltrating carcinoma positive for PAX8, suggestive of RCC. Immunohistochemical staining for PD-L1 showed extensive expression in tumor cells (tumor proportion score 95%). FoundationOne® CDx testing was performed on the biopsy specimen and revealed CDKN2A/2B loss and CDK6 and MDM2 amplifications.
The patient also underwent a percutaneous biopsy of her dominant pulmonary mass, which revealed malignant spindle cell neoplasm staining positive for PAX8 and AE1/3, consistent with sRCC in the setting of the known large left renal mass.
Given her poor risk stratification per the International Metastatic RCC Database Consortium (IMDC) criteria, the decision was made to initiate systemic treatment with 4 cycles of combination ipilimumab and nivolumab followed by maintenance nivolumab monotherapy. After 10 cycles of maintenance nivolumab, the patient exhibited a remarkable response radiographically, with shrinkage of her primary renal lesion to 3.0 cm in greatest dimension and residual equivocal regional lymph nodes measuring up to 9 mm in size (Figure 1C and 1D). Her anemia and hypercalcemia also resolved.
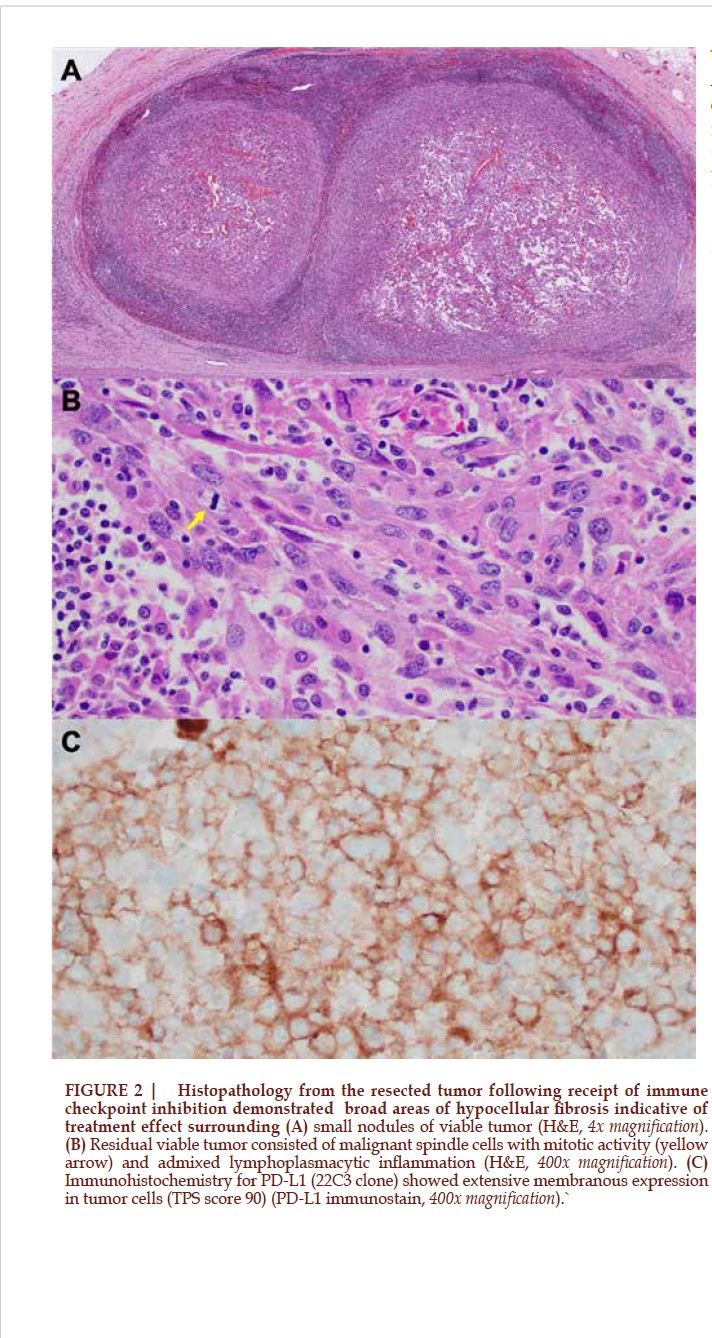
Following multidisciplinary discussion, given her favorable and durable response with low overall residual tumor burden, the decision was made to pursue cytoreductive nephrectomy, and given the small size and peripheral location of her renal mass, a robotic-assisted cPN with regional lymphadenectomy was performed. Estimated blood loss was 15 mL, and she was discharged uneventfully on postoperative day 1. Final pathology revealed ypT1aN0R0 ISUP grade 4 sRCC with extensive hyalinization from treatment effect (Figure 2). All margins were negative for carcinoma, and all fifteen sampled retroperitoneal lymph nodes were negative for tumor. The patient has since continued maintenance nivolumab for the past 6 months, on which she currently remains with no evidence of locoregional recurrence (Figure 1E and 1F) and no compromise in her renal function.
DISCUSSION
Our unusual case of metastatic sRCC in a young female highlights several unique aspects pertinent to the contemporary management of mRCC. In particular, we demonstrate1 a role for cytoreductive nephrectomy in select patients receiving ICI2, the safety and feasibility of a nephron-sparing and minimally-invasive approach to cytoreduction after downstaging with ICI3, the remarkable sensitivity of sRCC to ICI4, and the potential for ICI in improving candidacy for cytoreduction in even IMDC poor-risk patients, calling into question the applicability of validated prognostic models for mRCC in the current ICI era5. sRCC classically exhibits aggressive biology and often presents at a locally advanced or metastatic stage with a poor prognosis and limited response to targeted therapies6. The advent of novel ICI, however, has revolutionized the management of patients with metastatic sRCC, as evidenced by unprecedented response rates. Recent results from an exploratory post hoc analysis of long-term data from the phase III CheckMate 214 trial provided evidence that combination ipilimumab plus nivolumab yields a durable therapeutic response in patients with advanced clear cell RCC with sarcomatoid features6. These clinical observations are increasingly supported by emerging molecular evidence in sRCC.3,4
The role and timing for cytoreductive nephrectomy in mRCC have been a moving target over the past couple decades and continue to evolve1. The recent phase III non-inferiority CARMENA trial questioned the benefit of cytoreductive nephrectomy when combined with sunitinib, although numerous limitations were inherent to the study, and its applicability to the modern ICI era is debatable7. While we currently lack prospective evidence concerning the oncologic efficacy of cytoreductive nephrectomy in the setting of ICI, numerous retrospective institutional and national database studies have shown that nephrectomy after ICI is safe, feasible, and yields an astounding 10-20% complete pathologic response rate in the primary tumor (ypT0), with potential survival benefits2,8.
Together, the mounting evidence supports the paramount importance of patient selection in dictating appropriate candidacy for cytoreduction of the primary tumor.
While radical nephrectomy represents the gold standard approach to cytoreduction (cRN), the efficacy of cPN for mRCC is less well understood. Recent reports have suggested that cPN can offer similar oncologic control to cRN in patients with mRCC while preserving renal function and reducing the risk of cardiovascular morbidity and mortality9. In fact, some report a survival benefit to cPN when compared to cRN in patients with mRCC10. There are theoretical risks, however, to performing cPN in patients with mRCC, including a more challenging technical dissection due to surrounding tumor and treatment effects, potential tumor invasion into surrounding tissues, and the risk of inadequate tumor resection or multifocality. Nevertheless, in our index case, we have shown that cPN can be safely accomplished following receipt of ICI in a minimally invasive fashion with minimal morbidity to maximally preserve renal function while still achieving complete residual tumor resection. In this case, use of ICI prior to cPN was beneficial to downsize and downstage the primary tumor, thereby facilitating nephron preservation, while resolving the paraneoplastic manifestations of the cancer that would otherwise limit the patient’s candidacy to undergo cytoreduction.
CONCLUSION
We present a unique case of metastatic sRCC in a young female successfully managed with robotic-assisted cPN after exhibiting a remarkable response to combination ipilimumab and nivolumab. Our case highlights several aspects pertinent to the contemporary management of mRCC including the role for cytoreductive nephrectomy in selected patients, the safety and feasibility of a nephron-sparing and minimally-invasive approach to cytoreduction after downstaging with ICI, and remarkable sensitivity of sRCC—a classically aggressive entity—to ICI. Ongoing and future molecular studies will more precisely inform response to immunotherapy and guide multimodal management for patients with mRCC.
REFERENCE
# Corresponding Author: Nirmish Singla, MD, MSCS The Johns Hopkins School of Medicine, 600 North Wolfe Street, Baltimore, MD 21287. nsingla2@jhmi.edu